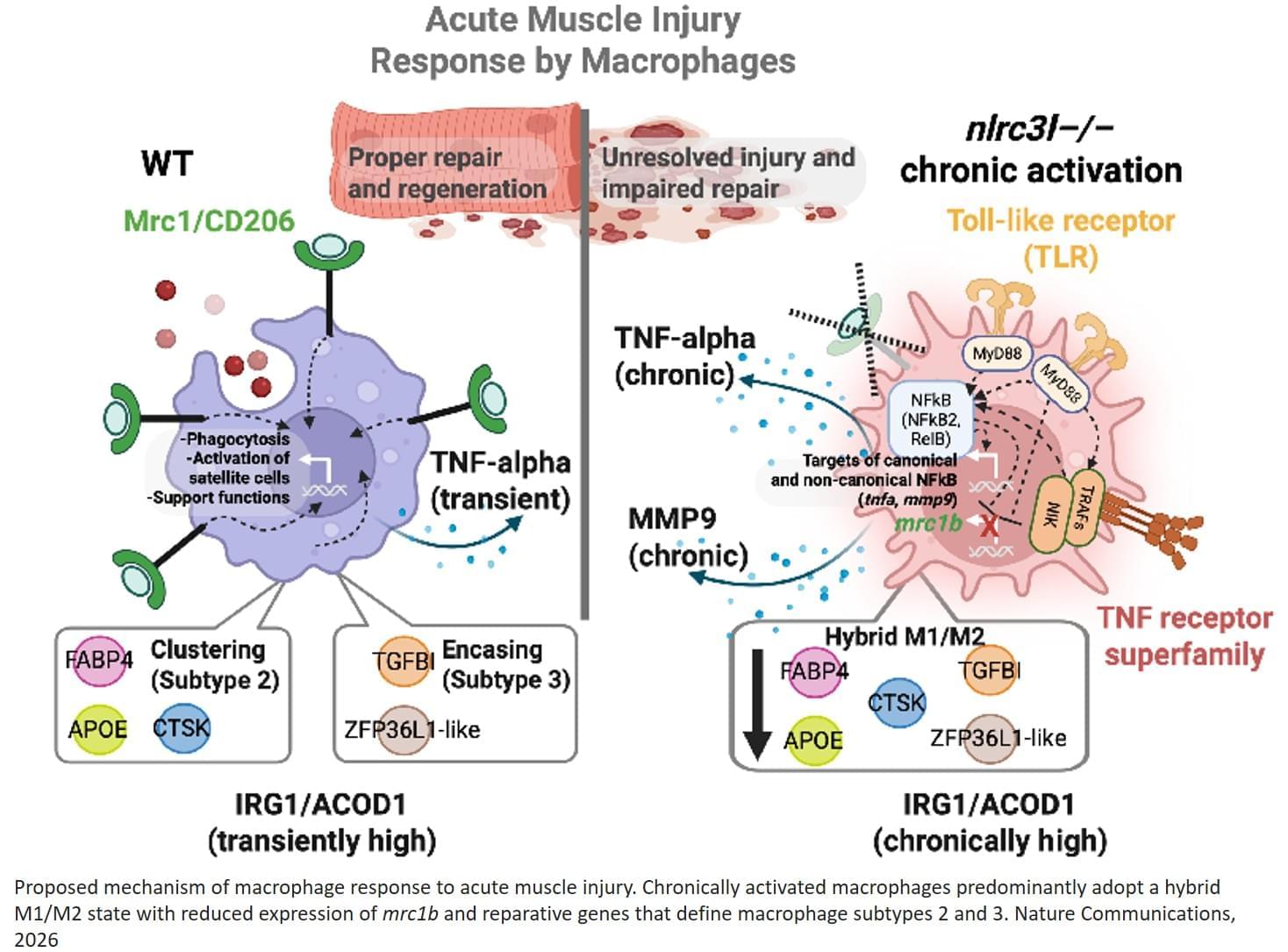
In recent years, mRNA in lipid nanoparticles (mRNA–LNPs) has emerged as a promising strategy for treating numerous conditions, including COVID-19, various cancers and chronic genetic disorders. To date, this technology has not been successfully used for pancreatic diseases, but that could be about to change. In a paper published in Nature, scientists from China report the development of a new lipid nanoparticle drug-delivery system specifically designed for the pancreas.
Lipid nanoparticles are a special class of fat-based carriers that encapsulate and deliver nucleic acids such as messenger RNA into cells. Among the reasons they have not worked for the pancreas until now is that most LNPs naturally accumulate in the liver and spleen. That means the therapeutic molecules they carry can’t accumulate to high enough levels to be beneficial.
However, the research team realized that while the liver and spleen are wrapped in a dense, protective outer layer called a capsule, the pancreas is only covered by a thin layer of connective tissue. They wondered if these organ capsules act as a biological filter. If so, they could perhaps design nanoparticles large enough to be physically blocked by the walls of the spleen and liver, leaving the pancreas as the only place to go. They named this discovery the capsule-filter-mediated pancreatic-targeted (CAMP) mechanism.