There are endless viruses in our midst, made either of RNA or DNA viruses, which exist in much greater abundance around the planet, are capable of causing systemic diseases that are endemic, latent, and persistent—like the herpes viruses (which includes chicken pox), hepatitis B, and the papilloma viruses that cause cancer. “DNA viruses are the ones that live with us and stay with us,” Denison said. “They’re lifelong.” Retroviruses, like H.I.V., have RNA in their genomes but behave like DNA viruses in the host. RNA viruses, on the other hand, have simpler structures and mutate rapidly. “Viruses mutate quickly, and they can retain advantageous traits,” Epstein told me. “A virus that’s more promiscuous, more generalist, that can inhabit and propagate in lots of other hosts ultimately has a better chance of surviving.” They also tend to cause epidemics—such as measles, Ebola, Zika, and a raft of respiratory infections, including influenza and coronaviruses. Paul Turner, a Rachel Carson professor of ecology and evolutionary biology at Yale University, told me, “They’re the ones that surprise us the most and do the most damage.”
Scientists discovered the coronavirus family in the nineteen-fifties, while peering through early electron microscopes at samples taken from chickens suffering from infectious bronchitis. The coronavirus’s RNA, its genetic code, is swathed in three different kinds of proteins, one of which decorates the virus’s surface with mushroom-like spikes, giving the virus the eponymous appearance of a crown. Scientists found other coronaviruses that caused disease in pigs and cows, and then, in the mid-nineteen-sixties, two more that caused a common cold in people. (Later, widespread screening identified two more human coronaviruses, responsible for colds.) These four common-cold viruses might have come, long ago, from animals, but they are now entirely human viruses, responsible for fifteen to thirty per cent of the seasonal colds in a given year. We are their natural reservoir, just as bats are the natural reservoir for hundreds of other coronaviruses. But, since they did not seem to cause severe disease, they were mostly ignored. In 2003, a conference for nidovirales (the taxonomic order under which coronaviruses fall) was nearly cancelled, due to lack of interest. Then SARS emerged, leaping from bats to civets to people. The conference sold out.
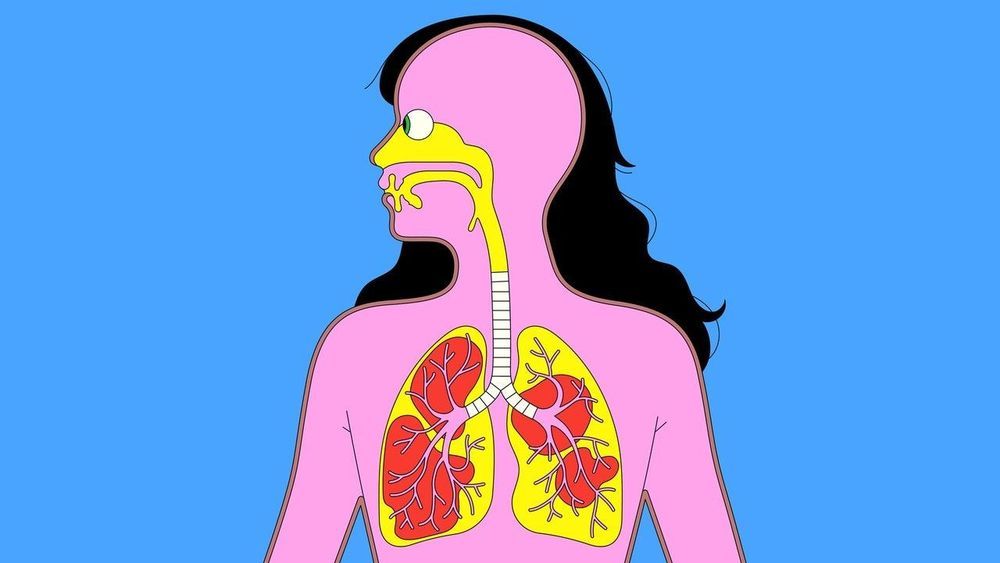
SARS is closely related to the new virus we currently face. Whereas common-cold coronaviruses tend to infect only the upper respiratory tract (mainly the nose and throat), making them highly contagious, SARS primarily infects the lower respiratory system (the lungs), and therefore causes a much more lethal disease, with a fatality rate of approximately ten per cent. (MERS, which emerged in Saudi Arabia, in 2012, and was transmitted from bats to camels to people, also caused severe disease in the lower respiratory system, with a thirty-seven per cent fatality rate.) SARS-CoV-2 behaves like a monstrous mutant hybrid of all the human coronaviruses that came before it. It can infect and replicate throughout our airways. “That’s why it is so bad,” Stanley Perlman, a professor of microbiology and immunology who has been studying coronaviruses for more than three decades, told me. “It has the lower-respiratory severity of SARS and MERS coronaviruses, and the transmissibility of cold coronaviruses.”