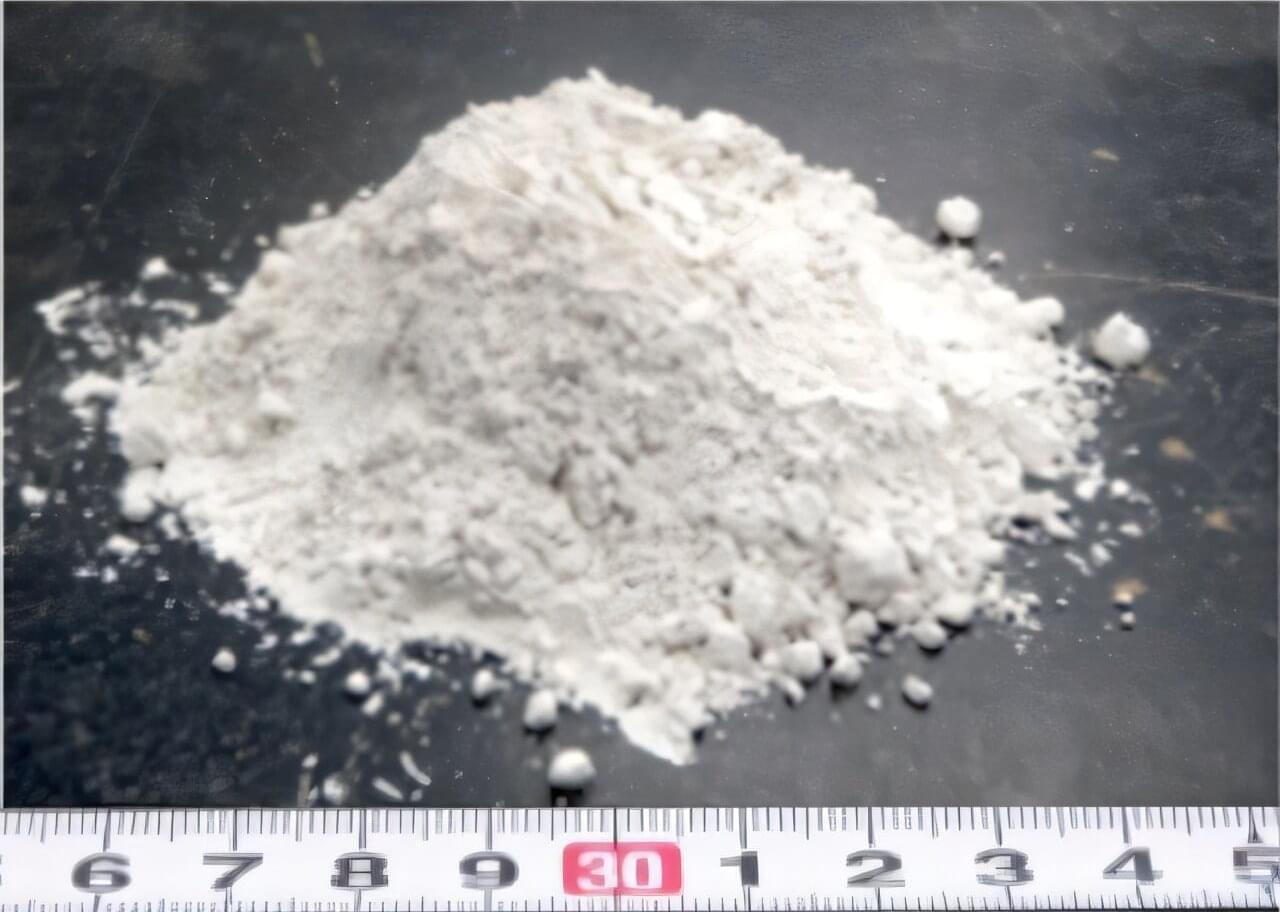
Pounding on the bottom of a glass bottle of ketchup is one of life’s small annoyances. Getting that sweet, red concoction from its solid phase to a liquid takes too long when you’re hungry and could even require messy strategies with a butter knife.
Now a team of scientists has shown that determining the point where the solid transitions to a liquid can be predicted from the properties of the solid phase alone. The research has been published in Physical Review Letters.
The new work focuses on yielding, a phenomenon where a solid-like material starts to behave like a liquid. “This behavior occurs constantly all around us, from desserts like custards that smoothly flow onto your spoon to personal care products like toothpaste that are easily squeezed out of tubes but hold their shape on your toothbrush,” Ryan Poling-Skutvik of the University of Rhode Island in the United States told Phys.org.