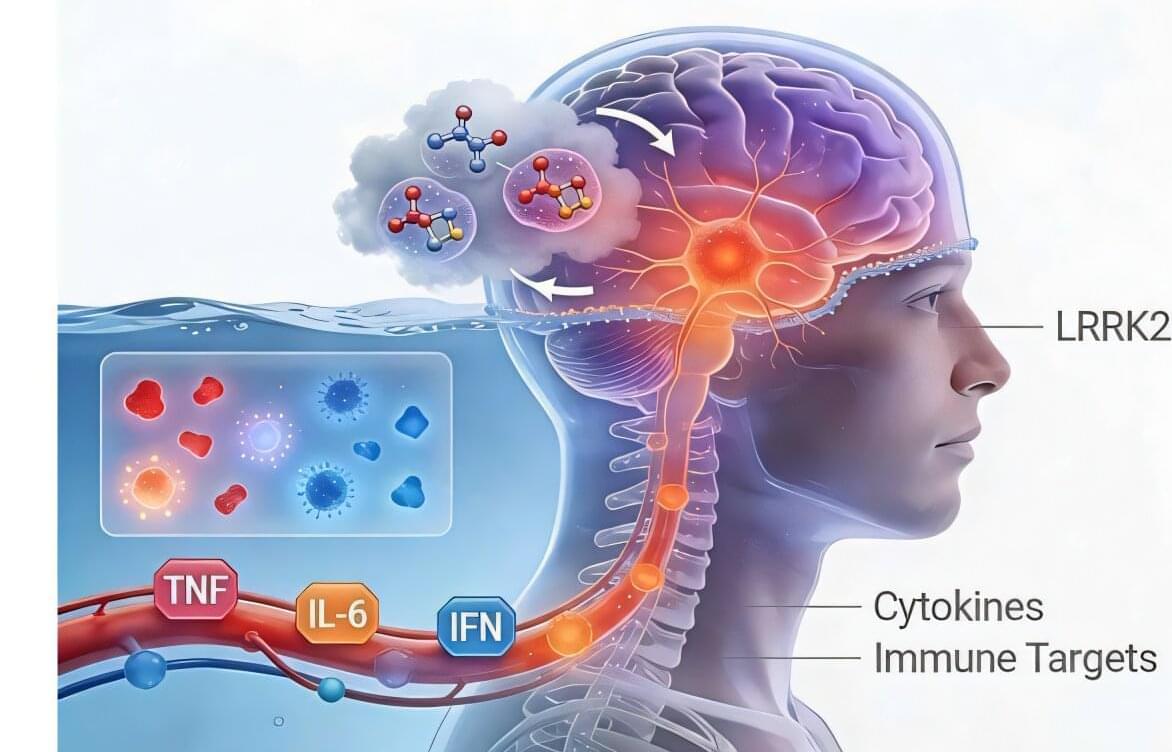
A study being conducted at The Hebrew University of Jerusalem, led by Professor Sagiv Shifman, found that many genes are essential for healthy brain cell development, but only a small share are currently connected to recognized neurodevelopmental disorders.
Read more from ynet here.
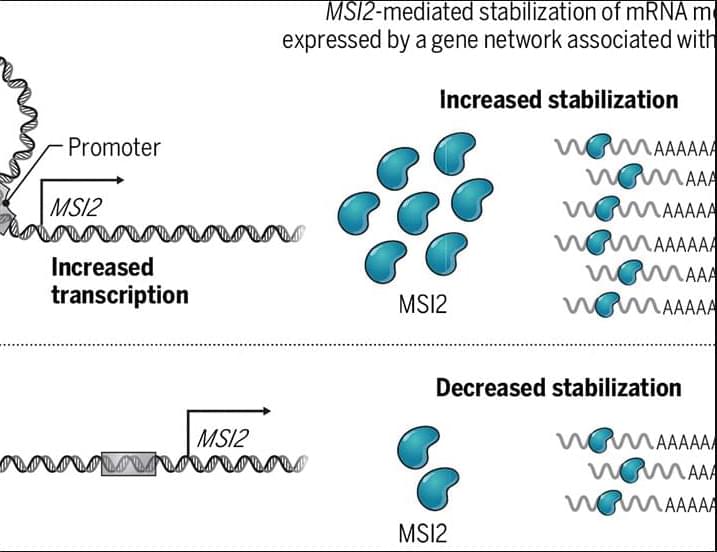
The researchers also identified clear patterns in how different genes contribute to disease. Genes that regulate other genes, such as transcription and chromatin regulators, were more often linked to dominant disorders, where a mutation in a single copy of a gene can cause illness. In contrast, genes involved in metabolic processes were typically associated with recessive disorders, requiring mutations in both copies of the gene.
To validate their findings, the team studied eight genes in mouse models — including PEDS1, EML1 and SGMS1 — and found major abnormalities in brain structure. In four of the cases, the mice developed microcephaly, a condition marked by an abnormally small brain.
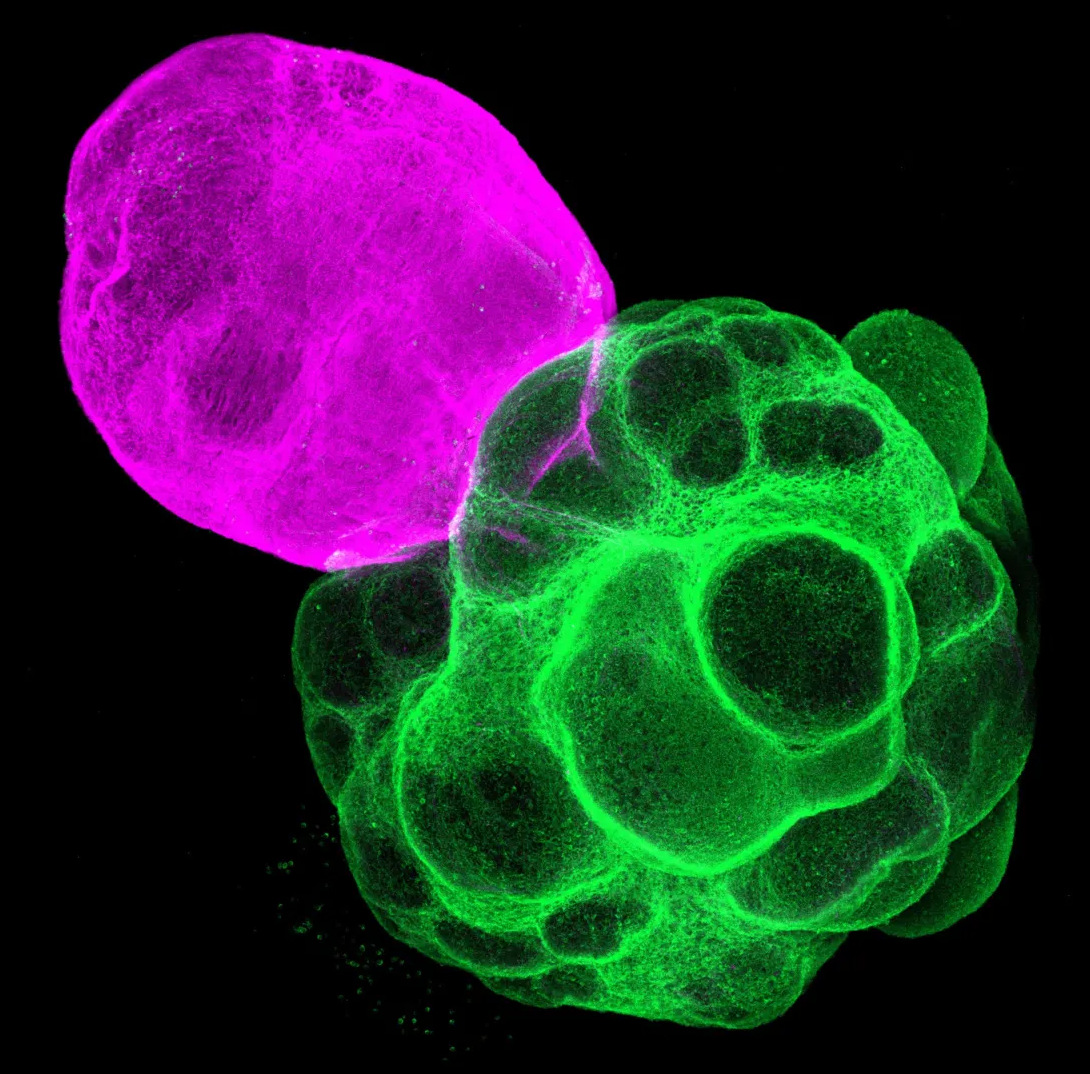
One gene, PEDS1, emerged as particularly significant. The gene plays a key role in producing plasmalogens, a class of lipids essential to cell membranes and nerve tissue. When PEDS1 was disabled in mice, brain cells exited the cell cycle too early and failed to properly differentiate and migrate, severely impairing brain development.